
02 Jan Understanding Ptotic Or Sagging Eyelids: Causes And Treatment Options
Changes to the appearance or position of the upper eyelids are a common concern for many individuals, particularly as time passes. In some cases, the upper eyelid may descend lower than its typical resting position. This is known as eyelid ptosis or a ptotic eyelid. While this change can occur naturally, it may prompt individuals to seek advice if it begins to interfere with vision or comfort, or if they would like more information about what it means for them personally.
Ptosis refers to a lowered upper eyelid margin and may occur on one or both sides. The condition can appear gradually or more quickly depending on the cause. It may be related to muscle function, connective tissue changes, or anatomical differences present since birth. For individuals in Perth and surrounding areas, learning more about eyelid ptosis can support clearer decision-making when considering possible treatment options.
Dr Guy Watts is a Specialist Plastic & Reconstructive Surgeon in Perth, Western Australia. He provides patient-specific assessments for individuals experiencing changes in upper eyelid position. His approach is focused on understanding the underlying cause and exploring treatment pathways where appropriate, with attention to both function and appearance.
What Is Eyelid Ptosis?
Eyelid ptosis describes a situation where the upper eyelid rests in a lower position than expected. This may affect one side only or be seen on both sides. Depending on its severity, ptosis may or may not affect the visual field. For some individuals, the change can be subtle and mostly noticed in photographs. For others, it may contribute to visual strain, tiredness, or a sensation of heaviness toward the end of the day.
It is important to distinguish ptosis from other conditions involving the upper eyelid. For example, excess upper eyelid skin (dermatochalasis), eyebrow position changes, or changes in upper facial structure can all influence how the eyelid appears. An accurate assessment helps identify whether the position of the eyelid margin itself is contributing to the overall concern.
In most cases of true ptosis, the change involves a key muscle in the eyelid known as the levator palpebrae superioris. This muscle is responsible for lifting the upper lid. If it becomes stretched, weakened, or detached from its normal position, the eyelid may no longer maintain its original height.
What Causes Ptotic Eyelids?
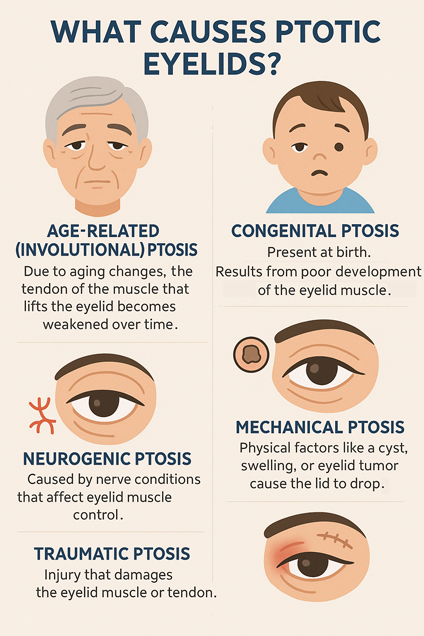
Several factors can contribute to ptosis. Identifying the likely cause plays an important role in guiding treatment recommendations. In his Perth clinic, Dr Guy Watts performs detailed assessments to understand each patient’s history, anatomy, and presenting features.
✓ Age-Related (Involutional) Ptosis
One of the most common causes of ptosis in adults is age-related change in the supporting tissues of the upper eyelid. Over time, the tendon that attaches the levator muscle to the eyelid margin can stretch or thin. This may lead to a gradual lowering of the lid, particularly toward the end of the day when muscle fatigue is more noticeable.
Individuals may become aware of this change when looking at photographs or during activities that require extended visual concentration. In some cases, people adjust their brow position subconsciously, which can lead to forehead tension.
Involutional ptosis typically develops in middle age or later, although it can occur earlier depending on individual factors such as anatomy, eye rubbing, or previous eye surgery.
✓ Congenital Ptosis
Congenital ptosis is present at birth and usually results from a developmental difference in the levator muscle. The muscle may not function normally, which affects its ability to lift the eyelid. This may be seen on one side or both.
In some cases, congenital ptosis may not affect vision. However, if the eyelid covers the pupil during early childhood, it may interfere with visual development. For this reason, early assessment is recommended, often involving both ophthalmology and specialist surgical input.
✓ Neurogenic Ptosis
This form of ptosis arises from nerve conditions that affect muscle control. Conditions such as Horner’s syndrome or third cranial nerve palsy can influence eyelid position. Another example is myasthenia gravis, which affects the communication between nerves and muscles.
In these cases, the eyelid position may vary throughout the day and may be accompanied by other changes such as pupil size, double vision, or overall muscle fatigue. Medical evaluation is essential when these signs are present.
✓ Mechanical Ptosis
In mechanical ptosis, the eyelid position is influenced by physical weight or restriction. This may result from a cyst, lesion, long-standing swelling, or previous injury. Over time, repeated irritation or inflammation in the upper eyelid may also contribute to structural changes that affect its position.
This form of ptosis may coexist with other eyelid changes and often requires careful assessment to determine whether treatment is appropriate.
✓ Traumatic Ptosis
Trauma to the eye or surrounding tissues may disrupt the normal function of the eyelid muscles or tendons. This can lead to a permanent change in eyelid position, depending on the severity and location of the injury.
In some cases, ptosis may also occur after previous surgical procedures involving the eyelids or upper face.
How Is Ptosis Diagnosed?
Diagnosis begins with a thorough consultation and physical examination. In his West Perth clinic, Dr Guy Watts takes a structured approach to assessing eyelid position, movement, and associated features.
As part of this process, the following elements are usually considered:
- Eyelid height: The vertical distance between the eyelid and pupil is measured and compared between both sides.
- Levator function: Eyelid movement is assessed to determine how well the levator muscle is functioning.
- Brow and skin position: Additional factors, such as eyebrow descent or upper eyelid skin redundancy, are evaluated to understand the broader picture.
- Photographs: Clinical images may be taken to assist in surgical planning or monitoring over time.
- Visual testing: If there is a concern that the eyelid is affecting the visual field, further testing may be arranged.
In cases where sudden onset ptosis or other symptoms are present, referral for neurological or ophthalmological assessment may also be recommended.
Blepharoplasty Surgery Before and After Photos
Photo disclaimer:
Each surgical procedure produces unique outcomes influenced by factors such as body composition, skin tone, laxity, age, and genetics. The before-and-after photographs displayed are of actual patients and are provided for informational purposes only.
Treatment Options For Ptotic Eyelids
Treatment depends on the cause of ptosis, the degree of change, and whether vision or comfort is affected. In some individuals, the change is stable and may not require treatment. In others, treatment may support both visual function and overall appearance.
Dr Guy Watts discusses all available options with patients in Perth, considering both surgical and non-surgical approaches.
✓ Non-Surgical Approaches
Non-surgical management is sometimes appropriate for mild ptosis or in cases where surgery is not the preferred option. These approaches may include:
- Observation: Monitoring the condition over time to assess whether further change occurs.
- Addressing underlying conditions: If ptosis is secondary to inflammation or neurological conditions, treatment of the underlying issue may help stabilise the eyelid position.
- Supportive eyewear: In rare cases, a small mechanical attachment known as a ptosis crutch can be fitted to glasses to support the eyelid.
It is important to note that non-surgical approaches do not reposition the eyelid but may assist with symptom management in select situations.
✓ Surgical Options
Surgery is considered when ptosis interferes with vision, contributes to physical strain, or is part of a broader decision regarding changes to the eyelids or upper face.
✓ Levator Advancement
This is the most common surgical technique used in adults with age-related ptosis. The levator muscle or its tendon is adjusted to elevate the eyelid to a more balanced position. The procedure is typically performed through a crease in the upper eyelid, which helps reduce visibility of the incision.
Surgery is planned to achieve symmetry with the opposite side while maintaining natural eyelid movement. During the procedure, adjustments are made based on the patient’s anatomy and pre-operative measurements.
✓ Frontalis Suspension
In cases where the levator muscle function is poor or absent, the eyelid can be connected to the forehead muscle (frontalis) using a sling. This allows the forehead to assist in lifting the eyelid. This approach is more commonly used in children or in complex adult cases.
✓ Combined Procedures
For some individuals, ptosis may occur alongside excess eyelid skin. In these situations, ptosis surgery can be combined with upper eyelid skin excision to address both concerns in a single operation. This approach is often used when the skin also affects vision or contributes to functional discomfort.
Recovery After Ptosis Surgery
Recovery varies from person to person but generally follows a progressive and well-supported course.
- Initial days: Mild swelling, bruising, or discomfort are expected. Cold packs and elevation of the head may help reduce symptoms.
- First week: Most patients return to light activities. Stitches are removed if non-dissolving sutures were used.
- Second week onwards: Swelling continues to settle, and the eyelid position stabilises further.
- One to three months: The eyelid continues to adjust as internal tissues settle. Final symmetry becomes more apparent.
Dr Guy Watts provides tailored aftercare to support healing and monitor progress, including recommendations on exercise after eyelid surgery to promote recovery and reduce swelling. Patients are encouraged to follow specific instructions regarding rest, activity, and eye care in the early recovery phase.
FAQs About Ptotic Or Sagging Eyelids
Do’s And Don’ts For Managing Ptotic Eyelids
Do’s
Do seek professional advice
An accurate assessment by a medical specialist is essential to identify the underlying cause and explore appropriate management options.
Do monitor changes over time
If you notice a difference in eyelid position, symmetry, or vision, documenting these changes with photographs can be helpful during consultations.
Do protect the eyes from UV exposure
Sun protection can support skin and tissue health around the eyelids, especially in Western Australia’s high UV environment.
Do follow post-operative instructions carefully
If undergoing surgery, adhering to care instructions supports healing and helps reduce post-surgical irritation.
Do allow time for recovery
Eyelid position continues to settle in the weeks following surgery. Patience during this period is important.
Don’ts
Don’t assume all eyelid changes are cosmetic
Some cases of ptosis can affect visual function or be related to underlying conditions. A medical evaluation is always recommended.
Don’t rub or stretch the eyelids
Frequent rubbing or pulling can place strain on the eyelid structures and may contribute to changes in position over time.
Don’t rely on cosmetic treatments for ptosis
Topical creams or cosmetic injections do not reposition the eyelid margin and are not appropriate for treating ptosis.
Don’t delay seeking assessment if vision is affected
If you experience changes in your field of vision or eye strain, an earlier consultation may be beneficial.
Don’t expect immediate symmetry
Even after surgery, eyelid height may take time to stabilise. Minor differences between sides are normal during recovery.
Supporting Informed Decisions
Changes in upper eyelid position can occur for many reasons and may affect individuals differently. For some, ptosis presents as a functional concern. For others, it may be part of a broader pattern of facial change over time. Understanding your options begins with a careful assessment and an open discussion about what you have noticed and how it affects you.
Dr Guy Watts is a Specialist Plastic & Reconstructive Surgeon based in Perth with a focused interest in eyelid conditions. He offers an evidence-based, individualised approach to assessment and treatment. His care philosophy is built on clinical knowledge, open communication, and patient-specific decision-making.
If you are seeking professional advice about ptotic eyelids, a consultation with Dr Watts can help you explore your options, understand your anatomy, and consider whether treatment is appropriate for your needs and goals.
Further Reading
- Read more about Dr Guy Watts’ Procedure Eyelid Surgery – Blepharoplasty
- Read more about Dr Guy Watt’s Blog on Does It Hurt to Get the Blepharoplasty Stitches Removed?
- Read more about Dr Guy Watt’s Blog on Can Blepharoplasty Affect Your Vision?
- Read more about Dr Guy Watt’s Blog on Sunken Eyes – Causes and Options
About Dr. Guy Watts – MED0001539378
FRACS (Plas) – Specialist Plastic Surgeon In Perth WA
Dr. Guy Watts is a Specialist Plastic Surgeon (AHPRA MED0001539378) with an extensive career that spans across renowned plastic surgery clinics worldwide. His experience has been honed through invaluable experiences at esteemed establishments such as the New York Eye and Ear Infirmary and the renowned Pitanguy Clinic in Brazil.
Having collaborated with the foremost cosmetic plastic surgeons on a global scale, Dr. Watts has chosen to return to Perth after a 17-year journey of intensive training and invaluable professional experience to bring the latest practices and technology in cosmetic plastic surgery to his patients.
Dr. Watts is a Fellow of the Royal Australasian College of Surgeons (FRACS) and a Member of the Australian Society of Plastic Surgeons (ASPS), Australasian Society of Aesthetic Plastic Surgeons (ASAPS) and the International Society of Aesthetic Plastic Surgeons (ISAPS).
Read about the potential Risks and Complications of Surgery
Read the Patient Information and Resources
About CLINISPA
Clinispa is Dr Watts’ bespoke medical clinic performing Cosmetic Aesthetic treatments. At Clinispa, we offer advanced clinical treatments in a luxurious and calming environment, tailored to support your skin’s health and appearance.
Clinispa aesthetic services are performed by Dr Guy Watts’ nursing professionals, who have a passion for and solid understanding of facial aesthetics.
All Clinispa clients are considered individually, with a personalised treatment plan consisting of advanced scientific approaches to cosmetic aesthetics. We incorporate innovative technologies in conjunction with superiorly formulated skin care.
For more information about the full range of Clinispa Aesthetic of Cosmetic Treatments visit the Clinispa website










Sorry, the comment form is closed at this time.